Monrovia, Liberia — Two years after the Unity Party (UP) government took office on a promise to “Unity Party (UP) Liberia’s collapsing health sector, the system remains trapped in a cycle of strikes, go-slows, and chronic dysfunction. The ongoing industrial action by specialized health workers—most notably nurse anesthetists—exposes not merely a wage dispute, but a deeper structural failure in health sector governance, fiscal prioritization, and post-donor transition planning.
At the heart of the unrest is a widening gap between government pronouncements and frontline realities. While the Boakai administration points to a US$16 million allocation in the FY2025 budget for salary enhancements as evidence of reform, health workers argue that the measures amount to incremental adjustments that fail to address structural inequities in pay, working conditions, and professional valuation.
Salary Reform in Name, Not in Substance
The government’s decision to establish a US$150 minimum wage for civil servants was politically popular, but analytically blunt. Specialized health professionals argue that the policy flattens wage structures without accounting for years of advanced training, technical risk, and professional scarcity. The case of nurse anesthetists is particularly instructive.
Earning an average gross salary of approximately US$600 per month—reduced to about US$400 after deductions—these specialists perform high-risk, life-saving procedures in an already fragile system. Their demand for a US$1,000 monthly salary is not arbitrary; it reflects prevailing regional benchmarks in countries such as Ghana and Sierra Leone. Against double-digit inflation, the government’s US$50 monthly top-up in late 2024 was widely perceived as symbolic rather than corrective, quickly eroded by rising food, transport, and housing costs.
The unresolved Salary Reclassification Policy—intended to align compensation with qualifications and responsibilities—has become a central fault line. Its delayed or uneven implementation has reinforced perceptions that reform is reactive rather than strategic.
The Donor Cliff and a Poorly Managed Transition
Compounding wage frustrations is the abrupt scaling down of USAID-funded health programs between mid-2024 and 2025. For years, Liberia’s health system functioned under a donor-dependent model, particularly for community health workers (CHWs). When external funding receded, the state proved unprepared to absorb these workers into the national payroll.
As a result, an estimated 30 percent of community health professionals reportedly experienced delayed or nonexistent pay, shortages of supplies, and the collapse of supervisory support. This donor “cliff” revealed a critical governance weakness: successive governments, including the current one, failed to plan a fiscally sustainable transition from aid dependence to domestic financing.
Beyond Wages: A Crisis of Working Conditions
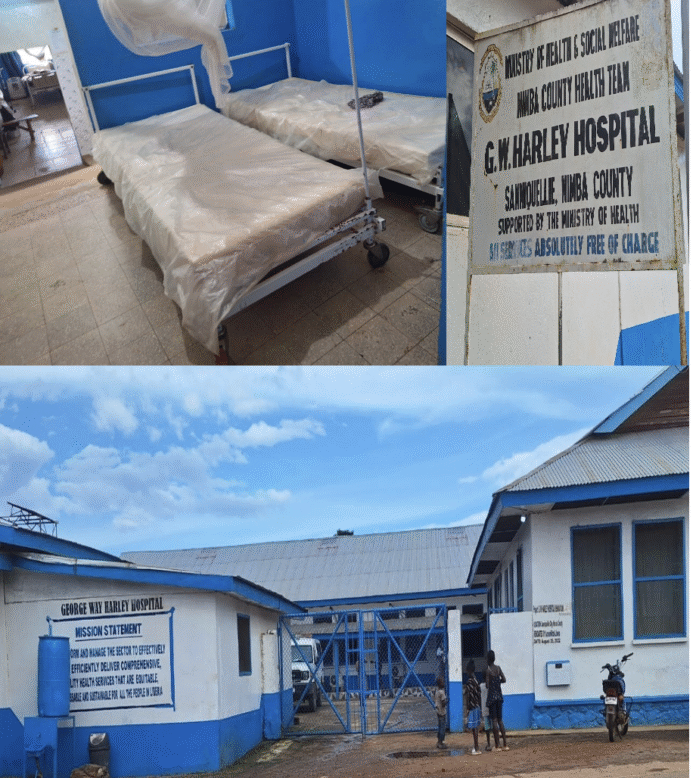
The strikes at ELWA Hospital and G.W. Harley Hospital underscore that compensation is only one dimension of the crisis. Health workers describe conditions that undermine both professional ethics and patient safety. Persistent shortages of basic consumables—gloves, sutures, anesthesia drugs—have reportedly forced cancellations of routine and emergency procedures. Infrastructure decay, marked by water shortages and erratic electricity supply at major referral hospitals, has turned already stressful workplaces into hazardous environments.
These deficiencies raise uncomfortable questions about budget execution, procurement efficiency, and institutional accountability within the Ministry of Health and its affiliated agencies.
Political Costs and Public Health Risks
Politically, the persistence of health sector strikes under the Unity Party threatens to erode the moral capital that accompanied its electoral victory. The administration campaigned on restoring dignity to public service and repairing the social contract; continued labor unrest suggests that this contract remains fragile, if not breached.
The consequences extend beyond politics. Liberia’s chronic brain drain—driven by salaries 40 to 50 percent lower than regional peers—continues unabated. More alarmingly, the current “go-slow” by just over 90 nurse anesthetists nationwide has immediate and deadly implications. With such a limited cadre, even partial work stoppages result in canceled cesarean sections, delayed trauma care, and preventable maternal and surgical deaths.
An Unfinished Rescue
The evidence suggests that Liberia’s health workers were not fully “rescued” but instead placed in a prolonged holding pattern—shielded from total collapse, yet denied a coherent path to recovery. Incremental pay adjustments, without comprehensive salary restructuring, reliable drug supply chains, and infrastructure stabilization, are insufficient to restore confidence or functionality.
Unless the government decisively implements salary reclassification, secures domestic financing to replace donor gaps, and addresses systemic procurement and infrastructure failures, the cycle of strikes is likely to persist. In the process, the greatest cost will not be political embarrassment, but the continued erosion of public trust—and the lives lost in a health system perpetually on the brink.